Electronic Health Records (EHRs) have revolutionized the healthcare industry by streamlining patient data, improving care coordination, and enhancing patient outcomes. However, the road to EHR implementation is not without its challenges.
In fact, according to a recent survey, only 30% of healthcare providers report that they are fully satisfied with their EHR system. Several obstacles can make EHR implementation daunting, from cost concerns to interoperability issues.
In this blog, we’ll explore some common challenges of implementing EHRs and provide you with strategies to overcome them.
EHR implementation requires significant financial and human resources, and the failure to understand the challenges can lead to cost overruns, low adoption rates, and decreased patient satisfaction.
By anticipating and addressing the challenges of EHR implementation, healthcare organizations can successfully transition to electronic record-keeping, improve operational efficiency, and ultimately provide better patient care.
Despite the many benefits that EHRs offer, healthcare organizations face several challenges when implementing these systems. Many factors can complicate the transition to electronic record-keeping, from financial considerations to staff training.
This section will explore six common challenges healthcare organizations may encounter during EHR implementation and discuss strategies to overcome them.
EHR implementation can be expensive, requiring significant financial resources for software, hardware, and staff training. Additional costs may include ongoing maintenance, upgrades, and compliance with changing regulations.
Healthcare providers and staff may resist the change to electronic record-keeping due to concerns about data security, privacy, and workflow disruptions. Resistance can lead to slow adoption rates and decreased productivity.
EHRs contain sensitive patient information, which is critical to protection. Healthcare organizations must implement robust data security measures to prevent breaches, comply with regulations, and maintain patient trust.
EHRs require staff to learn new skills and workflows, which can be challenging and time-consuming. Inadequate training can lead to low adoption rates and decreased productivity.
Healthcare providers often use different EHR systems, complicating data exchange and interoperability. Ensuring EHR systems can communicate with each other is critical for effective care coordination.
EHR implementation can disrupt existing workflows and decrease productivity as staff adjusts to new systems and processes. Healthcare organizations must develop strategies to minimize these disruptions and ensure EHRs enhance rather than hinder patient care.
Overcoming the challenges of EHR implementation requires careful planning and a commitment to addressing potential obstacles. This section will explore six strategies to help healthcare organizations successfully transition to electronic record-keeping.”
And here are the six strategies mentioned in the introduction:
Before implementing an EHR system, healthcare organizations should conduct a thorough cost-benefit analysis to evaluate the financial and operational impact of the transition. This analysis can help organizations determine if EHR implementation is feasible and identify potential cost-saving opportunities.
A comprehensive implementation plan is critical for successful EHR implementation. The plan should include clear timelines, roles and responsibilities, and strategies to address potential challenges.
Involving staff in the EHR implementation process can help build buy-in and support for the transition. Staff members can provide valuable feedback, identify potential challenges, and participate in developing workflows and processes.
Adequate training and support are critical for successful EHR implementation. Healthcare organizations should provide comprehensive training for all staff members, including ongoing training to ensure staff members are comfortable using the system.
Protecting patient data is critical during EHR implementation. Healthcare organizations must implement robust data security measures, such as encryption and access controls, to protect sensitive patient information.
Ensuring EHR systems can communicate with each other is critical for effective care coordination. Healthcare organizations should prioritize interoperability and data sharing to enhance patient outcomes and improve care coordination.
Sure, here are some examples of successful EHR implementations in healthcare organizations:
Engage clinical staff in implementing, including developing workflows and processes integrating with the EHR system. This can improve buy-in and ensure that the EHR system meets the needs of clinicians and patients.
Provide extensive training and ongoing support for all staff members to ensure they are comfortable using the EHR system. This can help reduce frustration and improve adoption rates.
Develop a comprehensive implementation plan with clear timelines, roles and responsibilities, and strategies to address potential challenges. This can help ensure the implementation process is well-organized and meets the organization’s needs.
Focus on collaboration and communication between IT staff and clinicians to identify and address issues quickly. This can help ensure that the EHR system is effective and efficient in meeting the needs of patients and staff.
Healthcare organizations can implement EHR systems and improve patient care delivery by following the above-mentioned strategies.
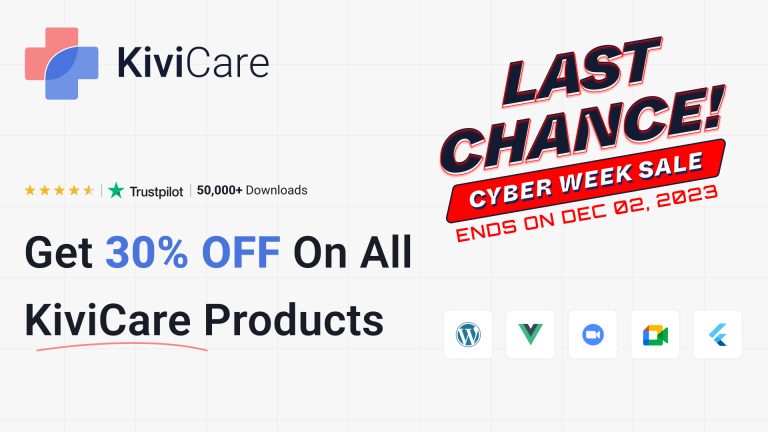
What are you waiting for? Take the FREE live demo TODAY!